正如我在上课时对大家所说:发表SCI 文章、尤其是高水平的文章,答复审稿者意见是关键,关系到一篇文章是否能被接受、是否能发表到高影响因子的杂志上。
针对答复审稿者的意见,大家普遍感到很困难,这种情况下,我们采用“实战”的方式,把我们组既往发表文章时,答复审稿者意见的原稿逐步发给大家,请大家对每篇都能详细去阅读,先反复看审稿者的问题,琢磨他们为什么要提出这样的问题,然后再看我们做的答复,有些答复很巧妙地避开审稿者故意“挖的坑”。希望能通过这种方式,使得大家在答复审稿者意见方面能逐渐得到提高。
按照我们上课时的顺序和发给大家的提纲,今天是第二篇:
《首发精神分裂症糖代谢异常与精神病理症状之间的关系》
一、这篇文章的思路比较 straightforward, 典型的case-control 设计,一组精神分裂症 (n=120) vs 一组正常组(n=31)。
二、指标包括:
1)糖和脂代谢指标+胰岛素(来自化验单);
2)病人检测PANSS。
三、结果:
1)比较两组之间的糖脂代谢指标差异;
2)在病人组,代谢指标是否与PANSS有某种关联。
这篇文章背后有两个有趣的小故事:
1)这篇文章的思路是在修稿另一篇文章时 (糖耐量试验 OGTT,准备在下一期发出) 产生的,那篇OGTT文章主要是比较服糖后2小时的血糖水平在精神分裂症病人与正常人之间的差异,当时我就想到:那么服糖前的基础水平如何呢?所以就有了统计分析和本文的产生。
2)文章写好后,我就投往Schizophrenia Research,因为这是一个计划外的文章,也没多考虑,就投往这个我比较熟悉的杂志,按我的经验,应该能比较顺畅地修回和接受,但未曾想到的是,文章直接被拒稿了!!难以置信啊!(同学们看看,即使对于张老师,被秒拒也是家常便饭,你们收到拒稿信时,不要灰心噢)。我痛定思痛、反复思考,然后毅然决然地决定:投稿到 Psychoneuroendocrinology。 这个真是太大胆决定了,要知道Psychoneuroendocrinology的影响因子远远大于Schizophrenia Research呀,被低影响因子杂志秒拒了,还竟然敢投稿高影响因子杂志??这就是你们张老师的艺高人胆大了:-))。幸运的是,这个Psychoneuroendocrinology主编比较友好,就给送审了哈。然后三个审稿者也比较nice, 就提出来一系列的苛刻建议来,让我又经历了一份痛苦的修稿过程。
好,言归正传,看我是如何答复三位审稿者意见,让他们欣然地接受了我们的文章。
下面是修改后的Cover Letter, 这部分是重点,可以先看,而且需要反复看:
Dear Editor,
Thank you very much for sending us the valuable comments of three reviewers on our manuscript (Ms. Ref. No.: PNEC-D-15-00458; Title: Glucose disturbances in first-episode drug-naïve schizophrenia: relationship to psychopathology), which have helped us to improve the quality of our paper greatly. We have thoroughly revised our manuscript according to the three reviewers’ helpful comments and suggestions. The comments and the critiques of the reviewers have been addressed and itemized as follows:
Question 1: The study should report correlations (even if not statistically significant) for the PANSS negative symptom scale as well .
审稿者提出对糖脂代谢指标与PANSS阴性症状的关联,即使是阴性结果,也要给出具体结果。
Answer: This point is excellent. Correlations for the PANSS negative symptom scale have been added to the second paragraph of the Results section on Page 7, showing as “A significant negative association between plasma glucose level and the PANSS positive symptom subscore was observed (r=-0.23, df=120, p=0.011) (Figure 1). However, neither significant association was found between glucose level and the PANSS negative symptom subscore (r=-0.09, df=120, p=0.22), nor between any other glucose and lipid parameters and the PANSS negative symptom subscore (all>0.05)”.
Question 2: In the discussion under “possible explanations”, the sentences regarding the first explanation are confusing and likely unnecessary – the results of this study are not explained by anti-psychotic usage if the subjects of this study have never been exposed.
类似这样的问题,不需要争辩,直接删除即可,因为不影响文章观点。
Answer: This point is very excellent. Indeed, the sentences regarding the explanation for the associate between antipsychotic usage and abnormal glucose metabolism in schizophrenia are confusing since our subjects in this study were drug naïve. These sentences have been deleted.
Question 3: In the methods section, it would be helpful to explain why the subjects of the study are anti-psychotic naïve – were the data collected at the initial evaluation for psychosis, shortly before anti-psychotics were started? Or was there some other reason that the patients did not have medication exposure?
很多老外教授对研究对象的背景细节要求很多,我们中国作者写文章时,往往对此写的比较简单。
Answer: The data were collected from these antipsychotic naïve patients at the initial evaluation for psychosis, shortly before antipsychotic were started. That means, after their first episode, they were admitted to the psychiatric hospital as inpatient. Then after the data had been collected, they were administered on antipsychotic medications. We have re-described these subjects in the Methods section on Page 4, under the subtitle- 2.1. Subjects, showing as: “One hundred and twenty FEDN inpatients were recruited at the initial evaluation for psychosis shortly before anti-psychotics were started. They were followed for about 3 months as inpatients after admission in order to establish a DSM-IV diagnosis of schizophrenia”.
Question 4: Did the investigators also measure early morning cortisol levels? Is it possible that cortisol abnormalities also contribute to the observed negative correlation between positive symptomatology and fasting plasma glucose levels?
这个问题常常是审稿者喜欢提出的,就是:与本研究中的生物学指标相关联的一些指标,但本文中又没检测,同时又不可能再去补实验或检测指标来,在这种情况下应该如何办?比较好办,最简单的方法就是在Discussion 的倒数第二段,作为一个limitation 列出来。或者是像在本文中这样,因为stress 对糖脂代谢影响比较大,就装模作样地先去讨论一番,这也显得对审稿者很尊重,然后再说,可惜我们没能去检测,是一种limitation。
Answer: This point is very excellent. Indeed, the stress and cortisol abnormalities may contribute to the observed negative correlation between positive symptomatology and fasting plasma glucose levels. Unfortunately, we did not measure early morning cortisol levels in this study, which has been added to the last paragraph of the Discussion section on Page 13 as one of limitations. At the same time, we have discussed more about the role of stress and cortisol in the observation negative correlation between positive symptomatology and fasting plasma glucose levels. Please read the last paragraph of the Discussion section on Page 11 and 12, showing as follows: A further consideration is the contribution of stress to the observed negative correlation between positive symptomatology and fasting plasma glucose levels, since a number of findings have demonstrated that stress may affect both the clinical symptoms of schizophrenia and the glucose metabolism (Lopuszanska et al 2014). Under the influence of stressors, there is increased activity of the hypothalamic-pituitaryadrenal (HPA) axis, resulting in hypercortisolemia, connected with the development of abnormal glucose metabolism and metabolic syndrome (Lopuszanska et al 2014). Stress-induced release of cortisol direct the processes of metabolism glycogenolysis in the liver and muscles, and gluconeogenesis in the liver and kidneys (Corcoran et al 2003). Also, previous studies showed that the high level of cortisol leads to hyperinsulinaemia, insulin resistance abdominal obesity and other components of the metabolic syndrome (Toalson et al 2004; Manoudi et al., 2012), and is a risk factor for type 2 diabetes (Brown et al., 2004). Moreover, in the case of patients with schizophrenia, hypercortisolism leads to increased accumulation of visceral fat, and impaired glucose tolerance (Toalson et al 2004). On the other hand, cortisol was found to be positively correlated with positive symptoms (Walder et al 2000), as well as with negative symptoms in schizophrenia (Zhang et al 2005). It should be pointed out that the experience of acute psychosis in schizophrenia patients was stressful itself. The physiological effects of this stress appear to be different in patients vs controls. It is possible, therefore, that stress may play a role in the negative correlation between positive symptoms and fasting plasma glucose levels in our present study. Unfortunately, we did not measure the early morning cortisol levels and 24-hour urinary cortisol. Further studies will need to evaluate the role of stress in our finding, for example, through the measurement of hormone level related to the hypothalamic-pituitary-adrenal axis. The data on plasma cortisol levels and its correlation to glucose levels and symptom scores would verify this viewpoint on the role of stress in psychosis.
Question 1: The interpretation of the findings exaggerates the importance of statistical differences. For example, there is no meaning in the difference between HOMA-IR’s of 1.21 and 0.81, because the cut off for insulin resistance is at least 5.
这个审稿者的这个意见有些过分了,实际上胰岛素抵抗的cutoff 点没有明确定义。但千万记住一点,不必要与审稿者进行争辩,顺着他/她的建议答复就可以了。
Answer: This point is excellent. Indeed, there is no meaning in the difference between HOMA-IR’s of 1.21 and 0.81, because the cut off for insulin resistance is at least 5. This interpretation of the findings exaggerates the importance of statistical differences, which has been added to the first paragraph of the Discussion section on Page 7 and 8, showing as “Our findings of higher levels of fasting plasma glucose and insulin, and potential insulin resistance in FEDN patient with schizophrenia is in accordance with a previous study (Ryan et al. 2003). However, it is worth noting that although there was significant difference in HOMA-IR with 1.21 for patients and 0.81 for healthy controls, there is no special meaning at this point, because the cut off for insulin resistance is at least 5. Moreover, it is unfortunate that the control cohort is much smaller than the patient cohort, which may lead to bias in the statistical analysis due to the imbalance in the sample size of two groups in our current study”.
Question 2: Other interpretations are not supported by the data. For example, the authors hypothesize that the patients had a greater amount of intra-abdominal fat than weight-matched control. These interpretation is not supported by the identical levels of triglycerides in the 2 groups.
看来这位审稿者不很友好,提出了过分的问题,但正如我在上面所说,不要同他/她争辩,顺着他/她答复就可以了,如果实在是不好答复,就放到limitation 里。
Answer: This point is excellent, which has been added to the Discussion section on Page 9 and 10, showing as “There are several possible explanations for the glucose metabolism abnormalities in schizophrenia. Firstly, ….. However, it is worthy of mentioning that the patients may have a greater amount of intra-abdominal fat than weight-matched control is only our speculation. Our finding of the identical levels of triglycerides in the 2 groups does not support this speculation. Further study investigating the abdominal body fat determined by magnetic resonance imaging and its relation to abnormal glucose metabolism in schizophrenia will be needed”.
Question 3: The patient group was studied during an acute episode of psychotic illness. Acute illness is associated with hypercortisolemia, which may have explained the increase in fasting glucose and corresponding (appropriate) increase in insulin levels. Unfortunately, the AM cortisol levels and 24-hour urinary cortisol were not measured. In the absence of such measurements, the study is not valid.
这个意见同第一位审稿者的意见类似,都谈到stress 对糖脂代谢影响的问题。这种情况下,把答复第一位审稿者的意见搬过来即可,但同时又专门列入一条 limitation。
Answer: These points are very excellent. Indeed, the patient group was studied during an acute episode of psychotic illness. Acute illness is associated with hypercortisolemia, which may have explained the increase in fasting glucose and corresponding (appropriate) increase in insulin levels. Unfortunately, we did not measure early morning cortisol levels and 24-hour urinary cortisol in this study, which has been added to the last paragraph of the Discussion section on Page 11 and 12 as one of limitations. Combining our answers to the Question 4 of the Reviewer 1, we have discussed in details about the role of stress and cortisol in the observation findings, showing as follows: A further consideration is the contribution of stress to the observed negative correlation between positive symptomatology and fasting plasma glucose levels, since a number of findings have demonstrated that stress may affect both the clinical symptoms of schizophrenia and the glucose metabolism (Lopuszanska et al 2014). Under the influence of stressors, there is increased activity of the hypothalamic-pituitaryadrenal (HPA) axis, resulting in hypercortisolemia, connected with the development of abnormal glucose metabolism and metabolic syndrome (Lopuszanska et al 2014). Stress-induced release of cortisol direct the processes of metabolism glycogenolysis in the liver and muscles, and gluconeogenesis in the liver and kidneys (Corcoran et al 2003). Also, previous studies showed that the high level of cortisol leads to hyperinsulinaemia, insulin resistance abdominal obesity and other components of the metabolic syndrome (Toalson et al 2004; Manoudi et al., 2012), and is a risk factor for type 2 diabetes (Brown et al., 2004). Moreover, in the case of patients with schizophrenia, hypercortisolism leads to increased accumulation of visceral fat, and impaired glucose tolerance (Toalson et al 2004). On the other hand, cortisol was found to be positively correlated with positive symptoms (Walder et al 2000), as well as with negative symptoms in schizophrenia (Zhang et al 2005). It should be pointed out that the experience of acute psychosis in schizophrenia patients was stressful itself. The physiological effects of this stress appear to be different in patients vs controls. It is possible, therefore, that stress may play a role in the negative correlation between positive symptoms and fasting plasma glucose levels in our present study. Unfortunately, we did not measure the early morning cortisol levels and 24-hour urinary cortisol. Further studies will need to evaluate the role of stress in our finding, for example, through the measurement of hormone level related to the hypothalamic-pituitary-adrenal axis. The data on plasma cortisol levels and its correlation to glucose levels and symptom scores would verify this viewpoint on the role of stress in psychosis.
Question 1: This manuscript is clear and well written, and is an interesting and potentially important study of glucose metabolism in first onset patients. To have recruited 120 first onset drug naïve patients is no small achievement and the size of the cohort should be emphasized more in both the abstract and introduction. This presents a major improvement over previous comparable studies. I would like to see the inclusion of some more details on the patient cohort, including duration of illness, the proportion of different subtypes of schizophrenia, PANSS and HAM-D scores (though HAM-D may be excluded, see below). The time period of sample collection should also be included, for both patients and controls. If the patient and control samples were collected during very different time periods this could be a limitation of the study. It is unfortunate that the control cohort is so much smaller than the patient cohort. However this should not affect the statistical analysis presented as t test/ANOVA is not affected by unequal sample size.
正如我在上面说的,很多老外教授特别注意研究对象的细节,这个审稿者就研究对象的细节问题也提出很多建议,比如:病程,病人亚型,PANSS总分及其亚量表的分数,以及对照组(n=31)与病人组(n=120)不平衡等。
Answer: Thanks for positive comments. These points are very excellent (这个审稿者是友军哈,意见比较positive,所以赶紧表扬一下,实际上这也是给主编看的,让他觉得我们的研究比较好).
1) Indeed, to have recruited 120 first onset drug naïve patients is very hard, with a lot of efforts. The size of the cohort has been emphasized more in both the abstract and introduction, showing as “Fasting glucose and lipid profiles, as well as homeostasis model of assessment-insulin resistance (HOMA-IR) index were determined in 120 never-medicated first-episode and 31 healthy control subjects matched for gender and age” (in Abstract). “In this study, we recruited a larger sample of FEDN patients (n=120)” (in Introduction).
2) Some more details on the patient cohort, including duration of illness, the proportion of different subtypes of schizophrenia, and PANSS (HAM-D has been excluded based on the suggestion of the reviewer, shown below) have been added to the Methods section on Page 4 and 5, under the subtitle- 2.1. Subjects, showing: “Their clinical subtypes were: paranoid, 64 (53.3%), undifferentiated, 44 (36.7%); disorganized 10 (8.3%); others 2 (1.7%). The patients had a mean age of 28.9±9.7 years (range: 16-49 year), and a mean duration of illness of 23.6±19.8 months”.
Also, the PANSS has been added to the Methods section on Page 5, under the subtitle-2.2. Clinical Measures, showing: “Mean scores on the PANSS were: positive subscore, 25.5±6.6; negative subscale, 19.3±7.8; general psychopathology subscale, 41.0±11.8 and total PANSS score, 85.8±19.9”.
3) The time period of sample collection has been included for both patients and controls in the Methods section on Page 5, under the subtitle- 2.3. Laboratory tests, showing:“Serum and plasma samples were collected following an overnight fast and at the same day when the clinical assessments were carried out in each subject. The patient and control samples were collected during the same time period”.
4) Indeed, the control cohort is so much smaller than the patient cohort. We have added this point as one of the limitations of the study to the first paragraph of the Discussion section on Page 7 and 8, showing: “However, it is worth noting that ……. Moreover, it is unfortunate that the control cohort is much smaller than the patient cohort, which may lead to bias in the statistical analysis due to the imbalance in the sample size of two groups in our current study”.
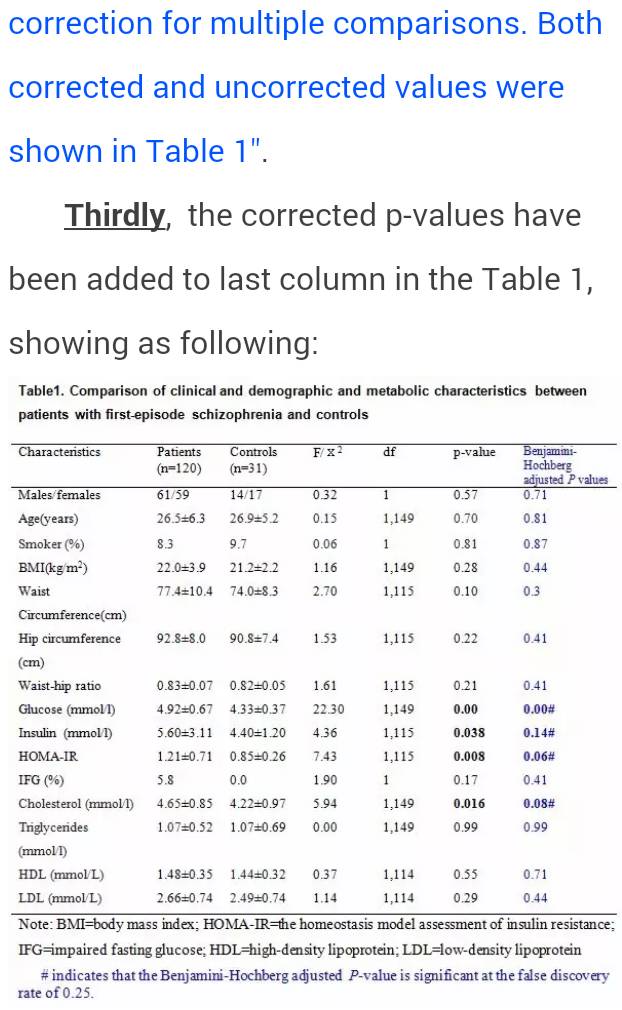
Question 2: The statistical analysis is adequate, however it seems a little pointless to perform Bonferonni corrections if no discussion is made of the results. Bonferonni may be an overly stringent correction where the repeated measurements are biologically connected e.g. members of the same pathway (as is the case in this study). A better alternative would be Benjamini-Hochberg, a less stringent way of controlling the false discovery rate. Both corrected and uncorrected values should be included in the data table. The PANSS analysis is interesting and the authors correctly state that this has not been previously attempted, presumably due to the small numbers in other studies. No results are presented for HAMD and I am not sure what this adds to an analysis of schizophrenia patients, except as a negative control. The purpose of this analysis should be clarified in the text, or omitted.
这位审稿者就统计方法提出问题,这也是比较常见情况,就是:常常审稿者对统计方法提出新建议和修改意见。这位审稿者认为Bonferonni校正过于严格,建议采用Benjamini-Hochberg方法, 当时我也不懂这个Benjamini-Hochberg校正,就重新上网查资料,同时学习了这个新的方法。说明:我的很多统计方法就是通过这种方式学习和掌握的。
Hopefully, we have made an appropriate revision based on the reviewers’ comments. Please let me know if there is anything else we need to do with the revision, and we’ll prepare it as soon as possible.
We thank you wholeheartedly for your excellent work. Your kind assistance is greatly appreciated. We look forward to any future correspondence.
Yours sincerely,
Xiang Yang Zhang, M.D., Ph.D.